

 Want to earn continuing education credit for this article? Learn more.
Want to earn continuing education credit for this article? Learn more.
Discover how massage therapists can help their clients with fibromyalgia break through chronic pain by addressing the practice of fear avoidance.
Affecting an estimated four million Americans, fibromyalgia is increasingly diagnosed in individuals with chronic pain disorders. Although fibromyalgia is admittedly a complex, physiological syndrome, there may also be an emotional component that keeps victims locked in a cycle of pain. Massage therapists who recognize when fibromyalgia clients fall into a harmful ‘fear avoidance’ pattern can better assist affected individuals in breaking the never-ending cycle of pain perpetuating fear, and vice versa.
About Fibromyalgia
Also referred to as fibromyalgia syndrome, fibromyalgia is a chronic arthritis-related syndrome primarily characterized by widespread muscle pain and tenderness. In the past the criteria for diagnosing fibromyalgia included checking 18 specific tender points on a patient’s body looking for pain elicited with pressure at 11 of these 18 sites. The problem was that this count rarely occurred in primary car where most diagnoses occurred and when it was performed it was done incorrectly as many physicians didn’t know how to correctly examine for tender points and some just refused to check.
Nowadays the American College of Rheumatology’s guidelines don’t require a tender point exam. Instead, the guidelines indicate that the main factor in diagnosing fibromyalgia is how long the pain has lasted and grading the pain using a widespread pain index (WPI), which is a measure of the number of painful body regions, along with a symptom severity (SS) scale.
The WPI is a measure from 0-19 where a patient would indicate where on their body they have had consistent pain for 3 months or longer.
- Left shoulder girdle
- Right shoulder girdle
- Left upper arm
- Right upper arm
- Left lower arm
- Right lower arm
- Left hip (buttock, trochanter)
- Right hip (buttock, trochanter)
- Left upper leg
- Right upper leg
- Left lower leg
- Right lower leg
- Left jaw
- Right jaw
- Chest
- Abdomen
- Upper back
- Lower Back
- Neck
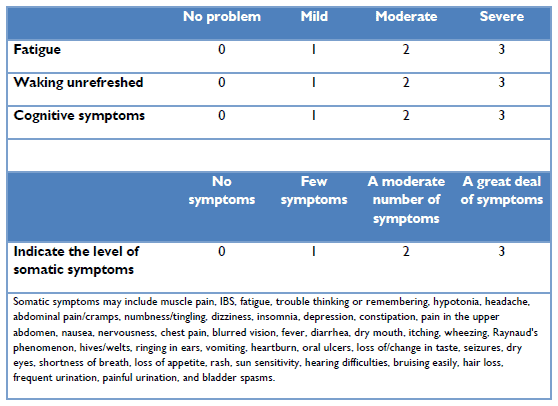
The SS scale is the sum of the severity of different symptoms whereby the final score will be between 0-12. This is scored as follows:
Physicians will determine if a patient meets the diagnostic criteria for fibromyalgia if the following three conditions are met:
- WPI ≥ 7 and SS scale score ≥5 OR WPI between 3-6 and SS scale score ≥ 9.
- Symptoms have been present consistently for at least 3 months.
- There is no other disorder that the patient has that would otherwise explain their pain.
Although these criteria may appear to be straightforward, there are many complicating factors involved with fibromyalgia. A handful of those factors include:
- Fibromyalgia can be a primary syndrome or it can be secondary to another autoimmune or rheumatic disease.
- Severe fatigue or a sleep disorder affects an estimated 90 percent of those with fibromyalgia.
- Fibromyalgia can manifest differently in each individual.
- Often times, a psychological component accompanies the physical aspect of pain in clients with fibromyalgia.
What Is Fear Avoidance?
 Fear avoidance is a psychological model that accounts for why certain clients may make the leap from acute to chronic pain. Fear avoidance suggests that it is overly fearful individuals who wind up suffering with chronic pain, to the degree that they avoid seemingly benign movement patterns so as to protect themselves from further pain.
Fear avoidance is a psychological model that accounts for why certain clients may make the leap from acute to chronic pain. Fear avoidance suggests that it is overly fearful individuals who wind up suffering with chronic pain, to the degree that they avoid seemingly benign movement patterns so as to protect themselves from further pain.
Developing fear avoidance after enduring significant physical pain is a logical emotional response. According to John Fry, PhD, a psychologist in Newport Beach, CA and board member of the National Fibromyalgia Association, “Nobody likes pain. You know how bad it’s been in the past, you know how it’s weighed you down, how you ended up in bed. You become fearful of moving around. You fear what it’s going to be like if it is an episode coming on.”
Studies have demonstrated that exercise can relieve fibromyalgia symptoms. However, patients fearful of their pain are frequently reluctant to work out or even move around much at all, knowing that such activity could reignite their pain. The body then loses its conditioning, which results in greater pain. Thus, the patient gets stuck in a cycle of being afraid of aggravating his or her pain, which causes more pain due to inactivity – which just serves to justify the fear of pain.
Helping Affected Clients
 First and foremost, compassion for those stuck in the fear-pain cycle is paramount. Because the path to fibromyalgia diagnosis often spans many years of suffering, those affected are likely to have been told their pain is all in their head. All too often, this patronizing cliché is spouted by practitioners who can’t explain the source of a patient’s pain.
First and foremost, compassion for those stuck in the fear-pain cycle is paramount. Because the path to fibromyalgia diagnosis often spans many years of suffering, those affected are likely to have been told their pain is all in their head. All too often, this patronizing cliché is spouted by practitioners who can’t explain the source of a patient’s pain.
Suffering from fear avoidance does not mean that a person’s pain is psychological. Instead, fear avoidance causes a de-conditioning of the body’s muscles, soft tissues and joints. The resultant inactivity is a physiological primer to musculoskeletal pain aggravation. Thankfully, helping ease clients’ fear of being active contributes to a reduction in their pain…as long as the therapist maintains respect and compassion for the client.
Here are some suggestions for helping fibromyalgia patients accept their pain (instead of fearing it):
- Explain that some treatments may cause some pain in the short-term, but will lead to long-term pain relief.
- Because there is no actual tissue damage with fibromyalgia, gentle, progressive exercise will not cause harm.
- Give your client access to studies showing that regular exercise/movement is the most effective means for relieving fibromyalgia-related pain.
- Work together on diaphragmatic breathing. Poor breathing practices can aggravate pain and contribute to fear.
- Acknowledge the fear that clients will feel discomfort when increasing their levels of activity, especially if they have been sedentary. However, insist on a graded, appropriate exercise plan for eventual pain relief.
- For those who remain stuck in fear avoidance, refer them to a cognitive behavioral therapist so that the client can confront their fears rather than be ruled by them.
Fibromyalgia is a complex, potentially agonizing pain syndrome. While the last thing someone with fibromyalgia needs is the additional musculoskeletal burden of being sedentary, the cycle initiated by fear avoidance can easily fuel a chronic pain cycle. Massage therapists with such clients can play an instrumental role in breaking this cycle – facilitating their freedom from fear and pain.
Earn continuing education credit for this article contained in our The Impact of Fibromyalgia series. Click here to enroll.















